+919790726189
This is your website preview.
Currently it only shows your basic business info. Start adding relevant business details such as description, images and products or services to gain your customers attention by using Boost 360 android app / iOS App / web portal.
Osteoporosis and Tooth Mobility: Understanding ...
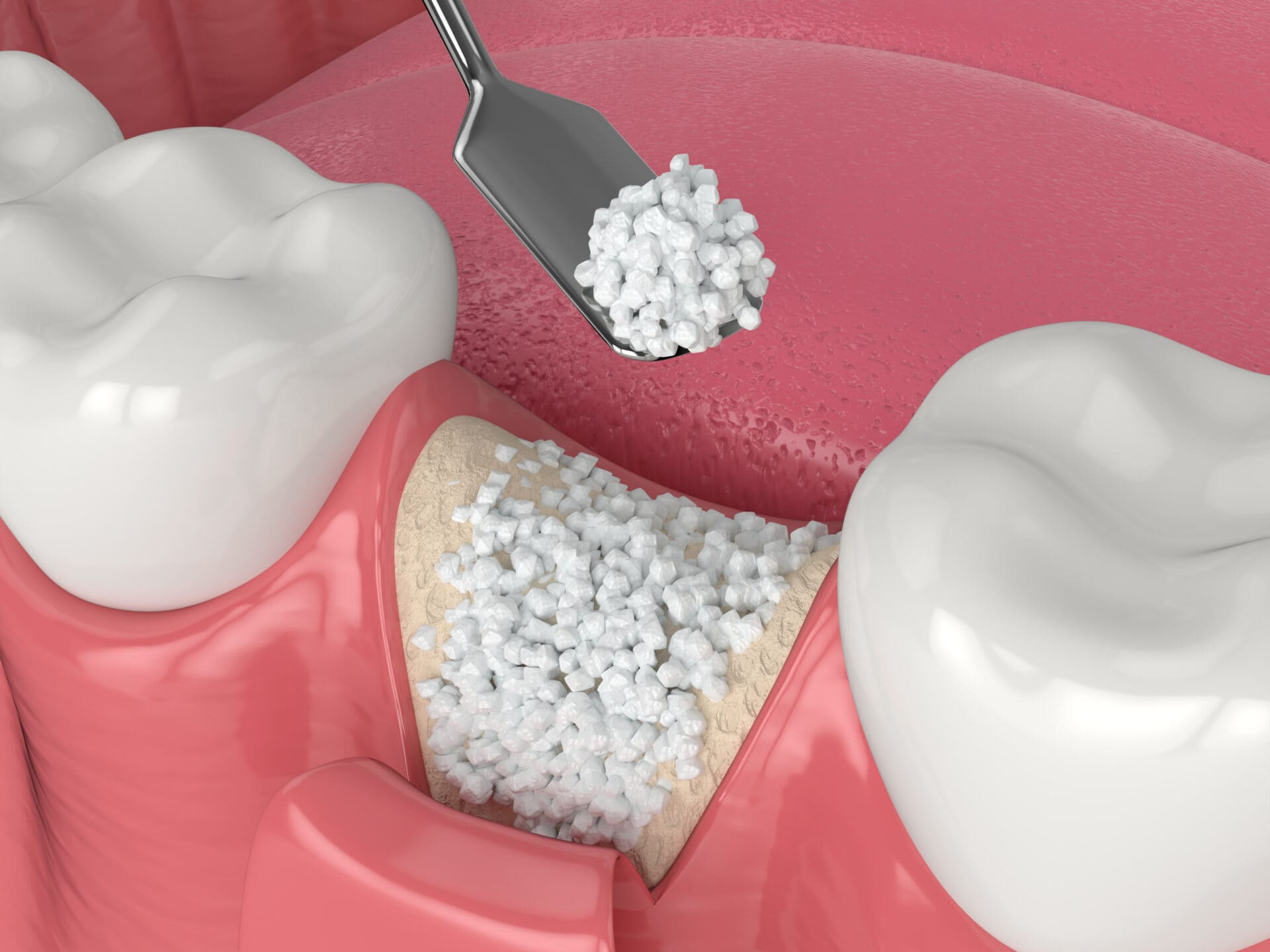
Osteoporosis and Tooth Mobility: Understanding the Connection@ Dr. Bharathi Dental Clinic and Implant Centre, West Mambalam Osteoporosis is a systemic bone condition that causes bones to become weak, porous, and more prone to fractures. It commonly affects the spine, hips, and wrists—but many people don’t realize that it can also impact oral health, particularly the stability of the teeth. One of the lesser-known but important consequences of osteoporosis is tooth mobility—a condition where teeth become loose in their sockets. How Are Osteoporosis and Tooth Mobility Related? Teeth are anchored to the jawbone by a structure called the alveolar bone. This bone provides support and stability to the teeth. In individuals with osteoporosis, the loss of bone density can extend to the jaw, causing resorption of the alveolar bone. As the jawbone becomes weaker and thinner, the teeth lose the firm support they require, leading to tooth mobility. Postmenopausal women are particularly at risk due to hormonal changes, especially the drop in estrogen, which plays a role in bone metabolism. When bone loss affects the jaw, signs may include receding gums, shifting teeth, and eventually, tooth loss. Symptoms and Signs to Watch For Loosening or wobbling of one or more teeth Receding gums or increased gaps between teeth Difficulty chewing or biting Changes in the way your teeth fit together Tooth mobility can also be worsened by gum disease (periodontitis), which is often more aggressive in people with low bone density. Therefore, osteoporosis can indirectly accelerate periodontal problems. Preventive Measures and Management If you are diagnosed with osteoporosis, informing your dentist is essential. A few key steps can help manage and prevent oral complications: Routine Dental Check-ups: Regular visits help in the early detection of bone loss and gum problems. Oral Hygiene: Daily brushing and flossing reduce plaque buildup and protect against gum disease. Diet and Nutrition: A calcium- and vitamin D-rich diet supports both skeletal and oral bone health. Medications: Certain medications for osteoporosis, like bisphosphonates, need special attention as they may have side effects related to the jawbone. Non-surgical Treatments: In cases of mild tooth mobility, splinting techniques can stabilize the affected teeth. Bone Density Testing: Especially in postmenopausal women and older adults, regular testing helps monitor osteoporosis progression. Osteoporosis is more than just a concern for bones—it has direct implications for your dental health as well. Loose teeth, shifting bite, and even tooth loss can result if osteoporosis affects your jaw. At Dr. Bharathi Dental Clinic and Implant Centre, West Mambalam, we emphasize a collaborative approach between your dentist and physician to monitor and manage both your systemic and oral health. Early detection and proper care can go a long way in preserving your smile and overall well-being. Dental Clinics in West Mambalam Dentists in West Mambalam Dentists in Ashok Nagar Best dentist near me Best Dental Clinics in West Mambalam Oral surgeon in West Mambalam Dental Implants in West Mambalam Oral surgeon in Ashok Nagar Painless tooth removal at West Mambalam Rootcanal treatment at West Mambalam Top rated dentist in West Mambalam

